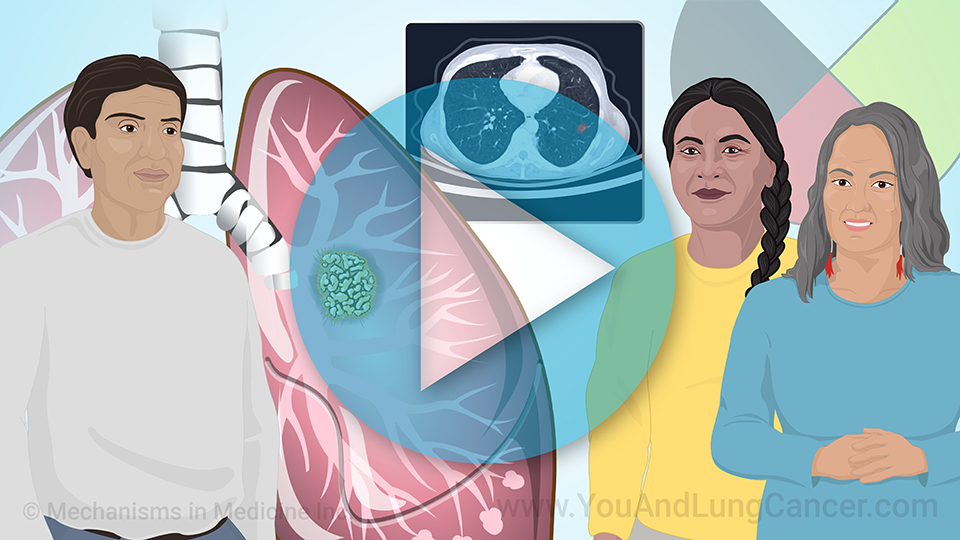
Understanding Immunotherapy for NSCLC with PD-1 and PD-L1 Biomarkers
*Please note: This slide show is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always consult your doctor about any questions you may have regarding a medical condition.
What is immunotherapy for NSCLC?
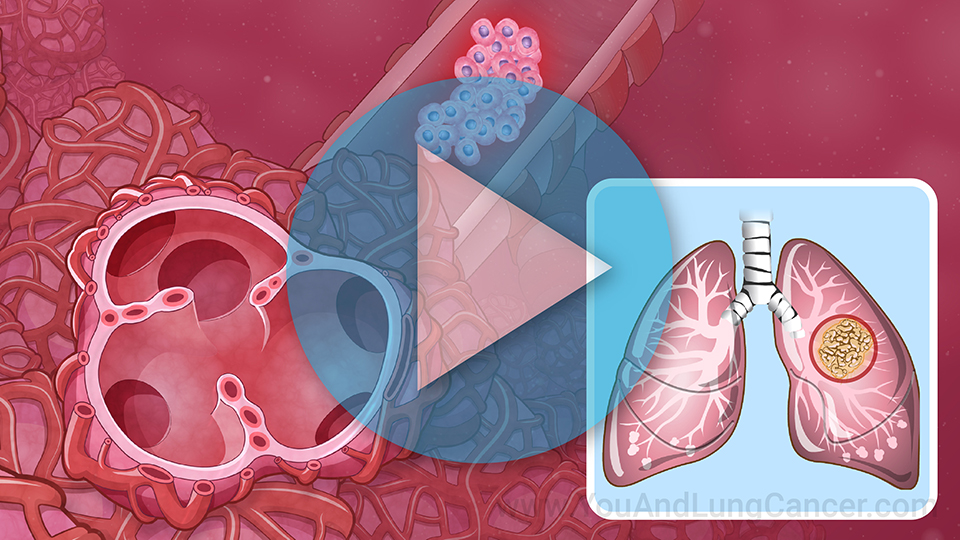
Immunotherapy is treatment that works with your body's immune system to fight cancer. The immune system's T cells normally catch and destroy abnormal cells, including cancer cells. But some cancer cells have features that let them get past the T cells.1
What is immunotherapy for NSCLC?
Immunotherapy keeps these features of abnormal cells from working, so your body's immune system can find and destroy them again. This slows the growth of cancer.
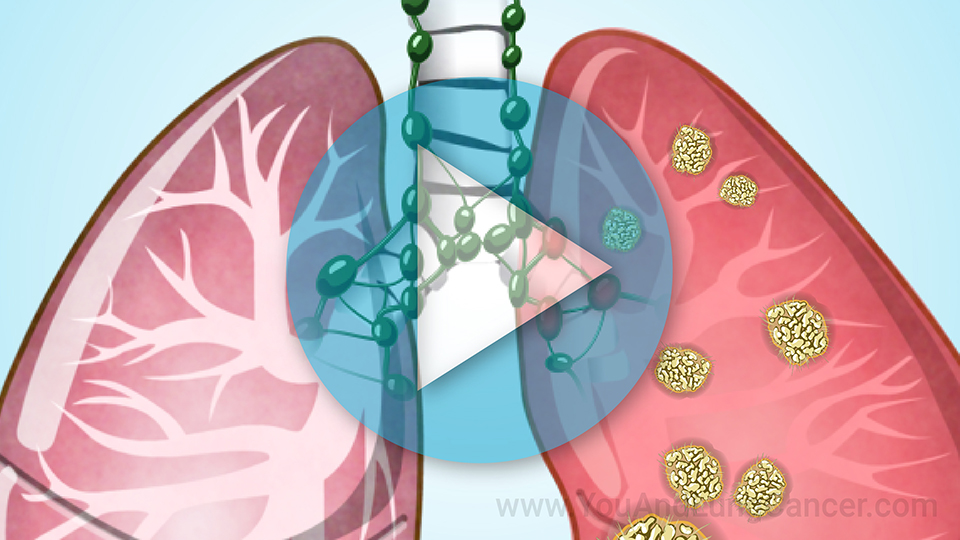
What are PD-1, PD-L1, and CTLA-4?
PD-1, PD-L1, and CTLA-4 are features that cancer cells use to slip past immune system checkpoints where they would normally be caught and destroyed.2
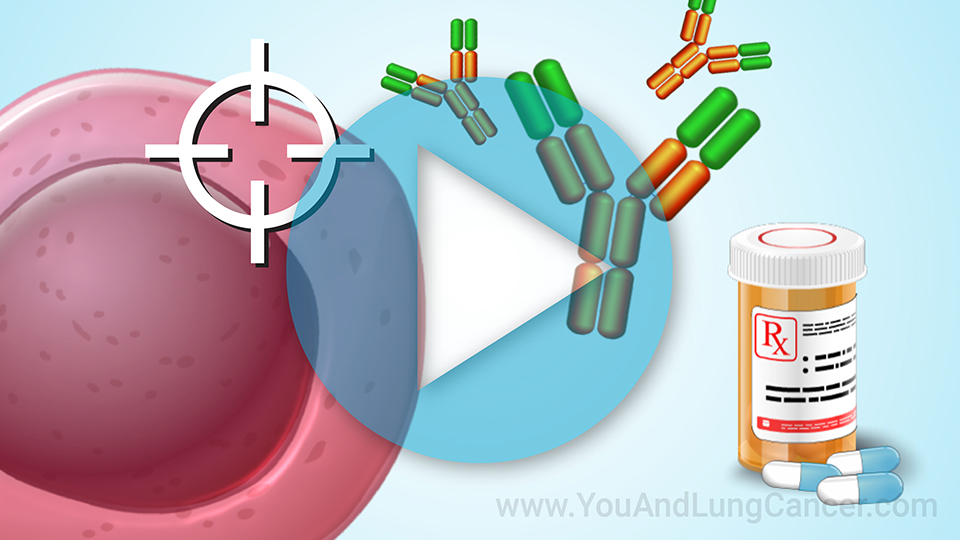
Why are checkpoint inhibitors used?
Drugs that help the immune system destroy cancer cells more effectively, without letting cells escape, are called immune checkpoint inhibitors. They are used when the body's immune system is being fooled by cancer cells looking and acting like normal cells.
What are PD-1 and PD-L1 inhibitors?
PD-1/PD-L1 inhibitors are drugs that target either PD-1 or PD-L1 and block their interaction. This slows or stops the growth of NSCLC.
What are CTLA-4 inhibitors?
Having CTLA-4 on a T cell can turn off the immune system's signal to destroy a particular cell. This is good if the cell is healthy, but bad if it is a cancer cell.
What are CTLA-4 inhibitors?
A CTLA-4 inhibitor helps by attaching to CTLA-4 and blocking it from working. This allows T cells to remain active and to destroy cancer cells.2
Checkpoint inhibitors for PD-1
Different medications work on different checkpoint proteins.
For example, drugs that target PD-1 include pembrolizumab (Keytruda®), nivolumab (Opdivo®) and cemiplimab (Libtayo®). You may take these drugs instead of chemotherapy, with it, or afterward.
Checkpoint inhibitors for PD-L1
Drugs that inhibit PD-L1 include atezolizumab (Tecentriq®) and durvalumab (Imfinzi®).2 These can also be given at different stages of treatment, sometimes with chemotherapy or other treatments.
Checkpoint inhibitors for CTLA-4
The drugs that target CTLA-4 receptors include ipilimumab (Yervoy®) and tremelimumab (Imjudo®). They keep T cells active to attack and destroy cancer cells, preventing the growth of the tumor.2
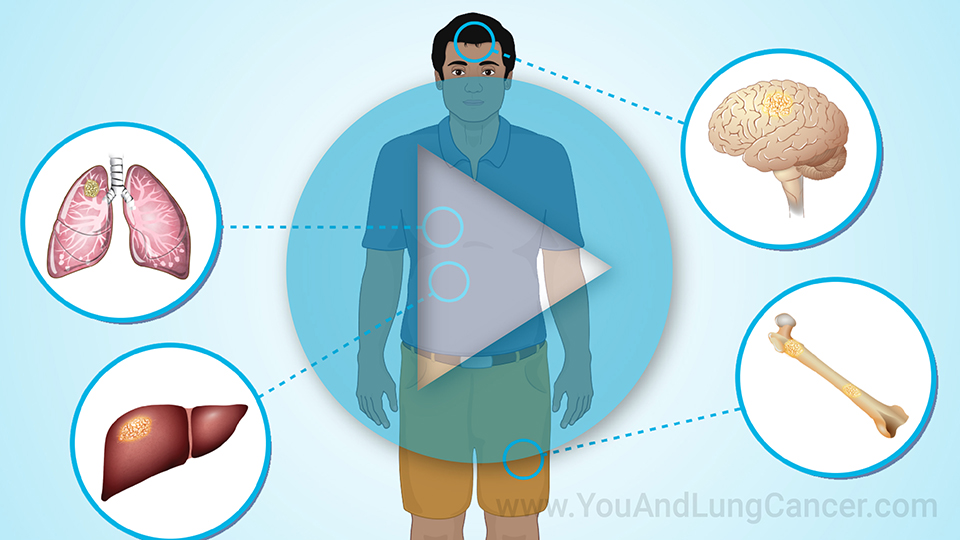
How are immune checkpoint inhibitors used in NSCLC?
Immune checkpoint inhibitors are used at different stages of NSCLC. They may be part of your first treatment, used later, or used for advanced cancer that has spread. You may have an immunotherapy drug alone, combined with a different one, or along with chemotherapy.
What if I have a driver mutation?
People whose cancer have the EGFR or ALK driver mutations, which drive the growth of cancer, do not usually receive immunotherapy because so far, immunotherapy is not effective in people with these mutations. In addition, targeted therapies are available that act on these mutations.1
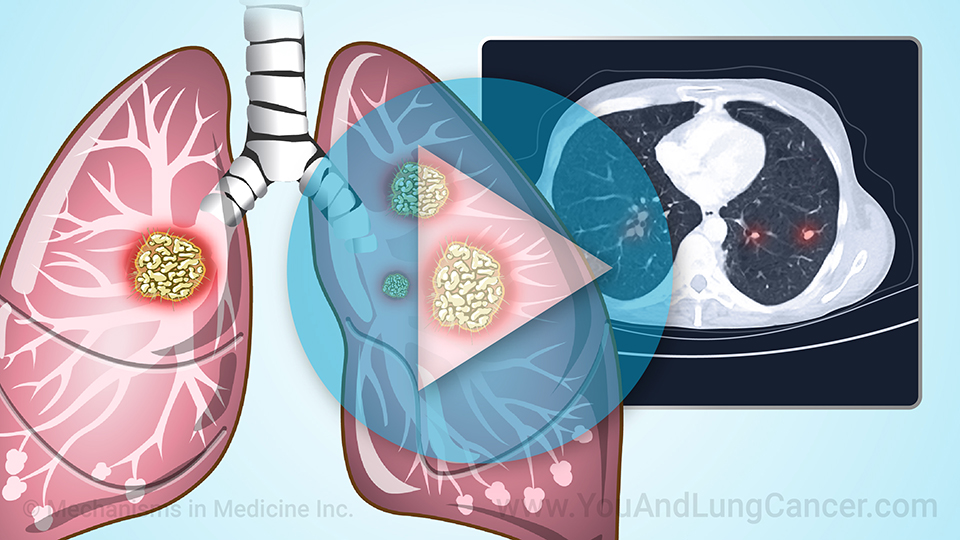
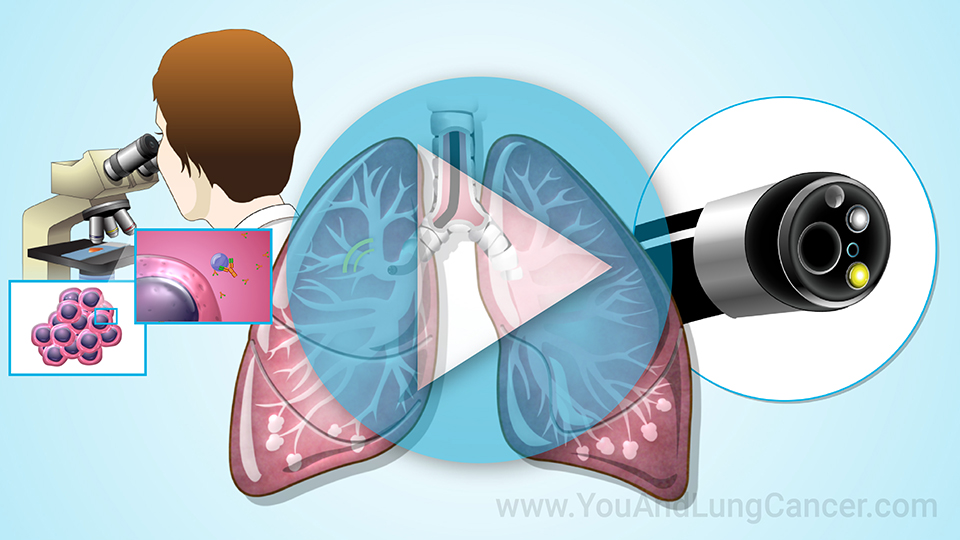
Biomarker testing and immunotherapy
The option of immunotherapy is one more reason why everyone diagnosed with NSCLC should have biomarker testing. Your cancer may be tested for PD-L1. Checkpoint inhibitors may work better in people with a lot of PD-L1, so this test will help your doctor choose treatment.
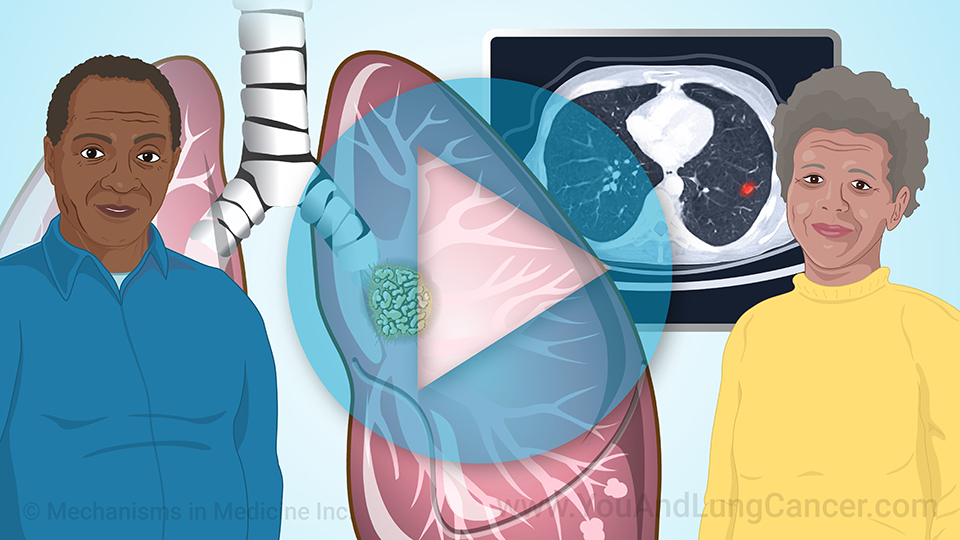
Immunotherapy drugs have made an important difference to many people with lung cancer, including advanced cancer, who are living much longer than they would have in the past.3
Biomarker testing and immunotherapy
Such specific features, or biomarkers, help determine the best treatment for your cancer, whether it is immunotherapy, a targeted therapy or something else.
Finding a clinical trial if you have PD-1, PD-L1, or CTLA-4
Clinical trials are an important way to learn if new treatments are effective in people with a disease like NSCLC, after they are proven to be safe.
If you have NSCLC, ask your doctor about clinical trials. A trial could give you a better outcome and the knowledge that researchers gain will help other patients in the future.
References
- American Lung Association. Lung cancer immunotherapy. Last revised: November 17, 2022.
https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/treatment/types-of-treatment/immunotherapy
- American Cancer Society. Immune checkpoint inhibitors and their side effects. Last revised: November 17, 2022.
https://www.cancer.org/cancer/managing-cancer/treatment-types/immunotherapy/immune-checkpoint-inhibitors.html
- Hellman M. How is immunotherapy for lung cancer changing the outlook for patients? Cancer Research Institute.
https://www.cancerresearch.org/cancer-types/lung-cancer
This slide show provides an overview of
immunotherapy for
non-small cell lung cancer (
NSCLC) with
PD-1 and
PD-L1 biomarkers. The option of immunotherapy is one more reason why everyone diagnosed with NSCLC should have
biomarker testing. Click through to learn about
PD-1,
PD-L1, and
CTLA-4 checkpoint proteins, and the different
immune checkpoint inhibitor drugs that act on PD-1, PD-L1, and CTLA-4. You can also learn about finding a
clinical trial if you have PD-1, PD-L1, or CTLA-4.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about lung cancer which will help other patients, caregivers and families.