Early Detection and Screening for Lung Cancer in Native Americans
*Please note: This slide show is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always consult your doctor about any questions you may have regarding a medical condition.
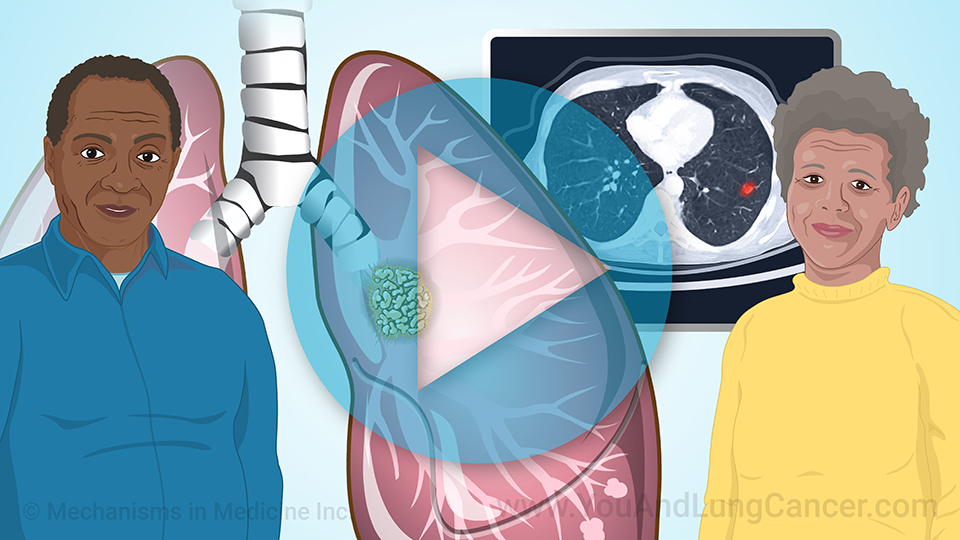
Why is screening for lung cancer important?
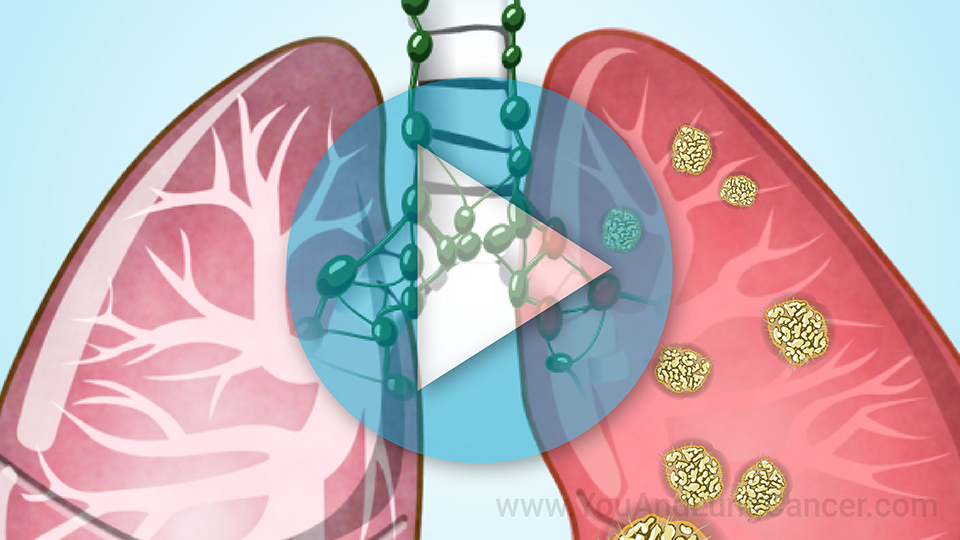
Lung cancer is more likely to be cured when it's detected very early. At early stages, patients often don't have symptoms. Screening is a way to detect lung cancer at this early, curable stage.
Why is screening for lung cancer important?
In a large study, screening found more than half of lung cancers before the patient had any symptoms.
Why are Native Americans less likely to be screened for lung cancer?
Compared with White Americans, Native Americans are:
- Less likely to be screened for lung cancer
- More likely to:
- Not know about lung cancer screening
- Not have health insurance
- Live far away from a screening facility
Why are Native Americans less likely to be screened for lung cancer?
Native Americans may also be less likely to get screened for lung cancer because of mistrust of the medical system. Because of racism and past abuses, such as the forced sterilization of Native American women, Indigenous people often don’t trust doctors.
Tobacco is culturally important for many Native American communities
Traditionally, many Native American communities use tobacco in medicinal and spiritual ceremonies. It's considered a sacred gift of the earth and a symbol of peace and healing.
Tobacco is culturally important for many Native American communities
However, the makers of commercial tobacco products have exploited the cultural importance of tobacco to Native Americans. As a result, Native Americans use tobacco more than any other racial or ethnic group in the United States. Smoking is the number one risk factor for lung cancer.
Lung cancer is a major health problem among Native Americans
Lung cancer is a leading cause of death from cancer among Native Americans. Compared with White Americans, Native Americans are more likely to be:
- Diagnosed with lung cancer before age 60
- Diagnosed with late-stage lung cancer
Benefits of lung cancer screening for Native Americans
The bottom line is: For Native Americans at high risk for lung cancer, screening can save lives – and the best time to get screened is before you feel sick.
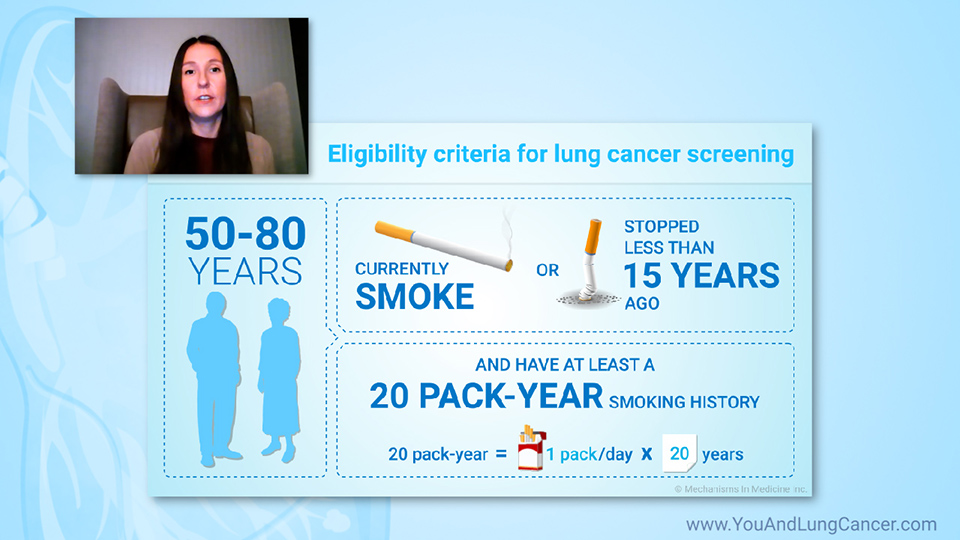
Who’s eligible for lung cancer screening?
You're eligible for lung cancer screening if:
- You're between 50 and 80 years old; and
- You currently smoke, or you quit less than 15 years ago; and
- You've smoked a pack a day for 20 years or two packs a day for at least 10 years; and
- You have no symptoms that could be caused by lung cancer.
Symptoms that could be caused by lung cancer
Symptoms that could be caused by lung cancer include:
- A cough that doesn't go away
- Chest pain
- Shortness of breath
- Coughing up blood
- Feeling tired all the time
- Losing weight without a known cause
If you're eligible for lung cancer screening, you'll get the most benefit if you have the test once a year.
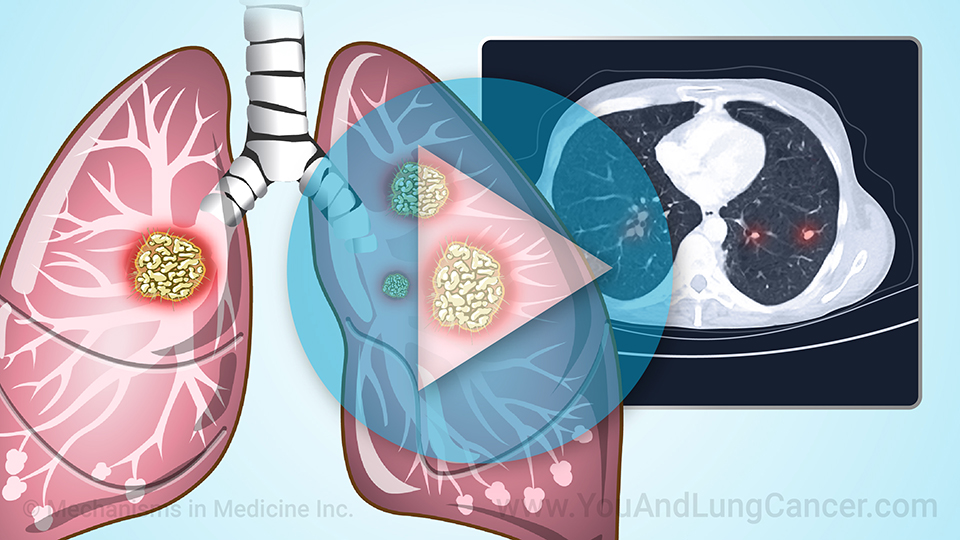
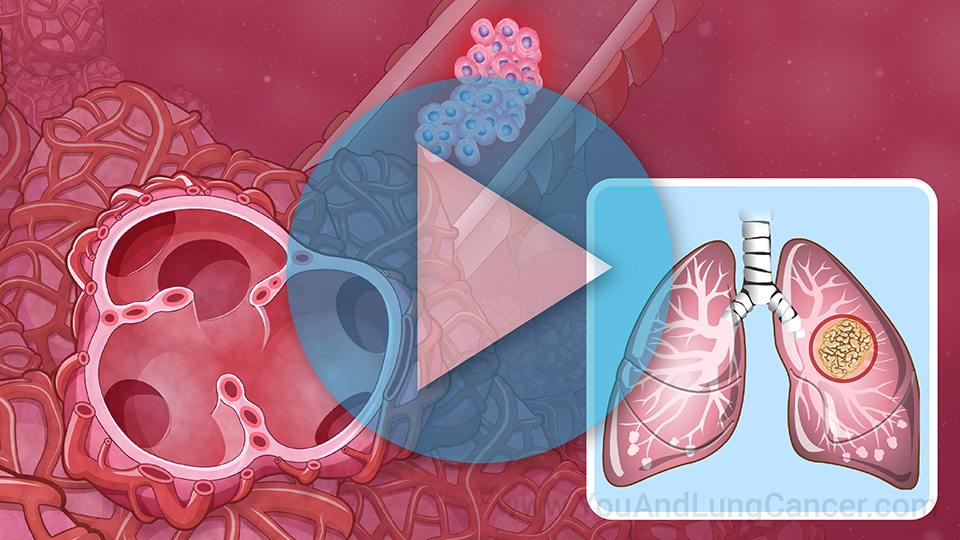
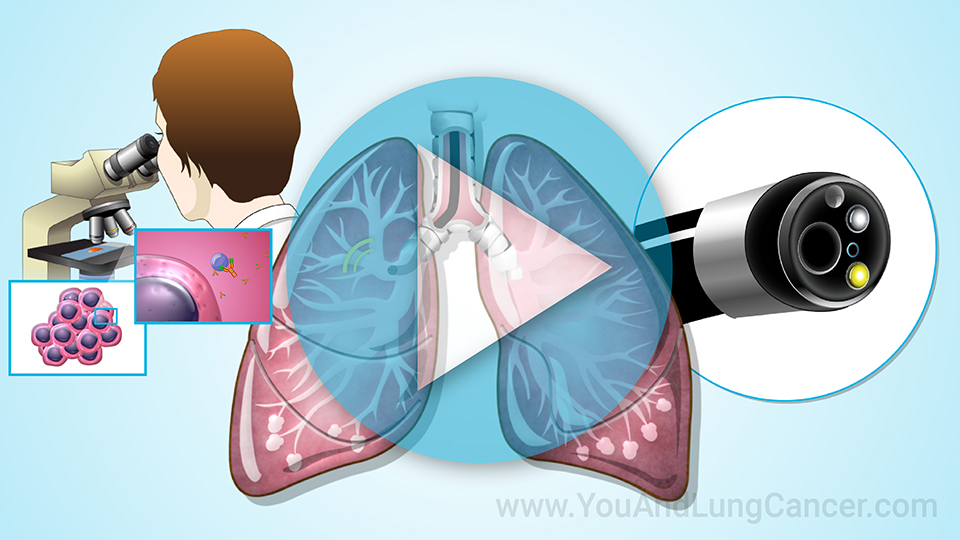
What happens in a lung cancer screening test?
The test is done with a CT scanner and is quick and painless. You lie flat on a table while the scanner takes dozens of pictures. A computer then converts the pictures into detailed images of your lungs.
What happens in a lung cancer screening test?
You don’t need to fast, get injections, or do any other preparation for the test. You will need to remove any metal you’re wearing, such as jewelry or a watch. If you’re feeling sick, you’ll need to reschedule the test for when you feel better.
Will health insurance pay for lung cancer screening?
Medicare and most private health insurance plans will pay for lung cancer screening.
If you’re on Medicaid, you’ll need to ask whether your state covers it, as coverage varies state-by-state.
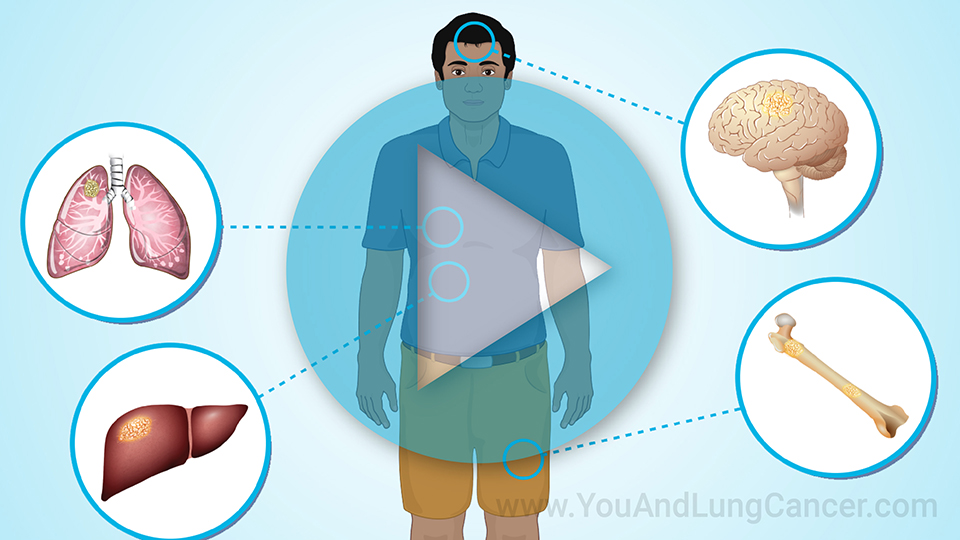
What are the risks of screening for lung cancer?
Like any medical procedure, a low-dose CT lung cancer screening test has some risks:
-
It involves a very small amount of radiation – about as much as everyone gets in 6 months from exposure to Earth's natural background radiation.
-
If the scan finds something, you may need additional imaging tests to find out if it's cancer.
- In rare cases, the scan may find something that looks concerning outside of the lungs. If this happens, you may need additional tests to check it out.
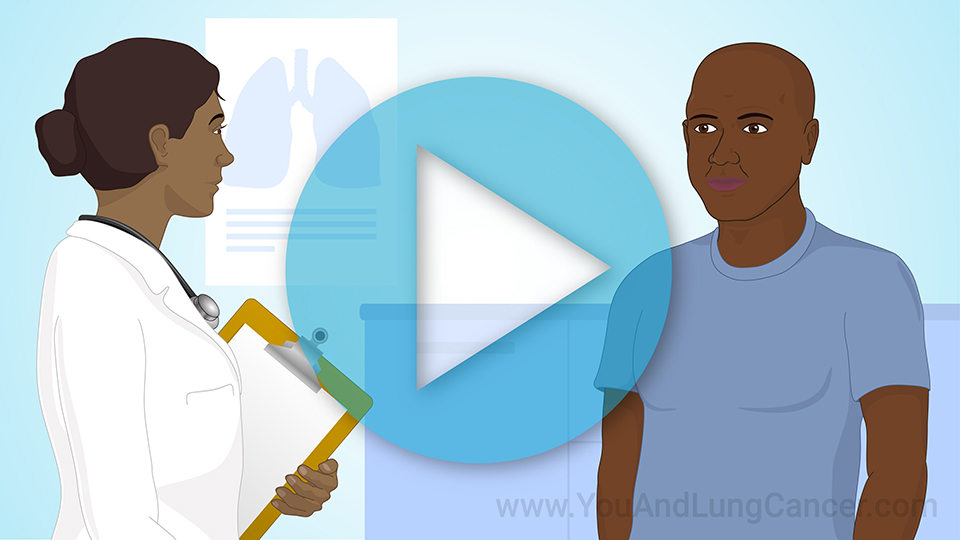
Questions to ask about lung cancer screening
Don't hesitate to ask questions about screening for lung cancer. Here are some questions you might have:
- Why should I get screened when I don't feel sick or have symptoms?
- Where should I go for screening?
- How long will it take to get my results?
- Will someone explain the results to me in language I understand?
- What are the next steps after I have the test?
Talk to a trusted healthcare adviser today!
Talk to a trusted healthcare adviser today about screening for lung cancer. Ask if it's right for you and where you can go to get it.
If you smoke, ask about getting help to quit. You'll get the most benefit from lung cancer screening if you also quit smoking.
References
- American Cancer Society. Lung Cancer Early Detection, Diagnosis, and Staging. Last revised: January 18, 2023.
https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/detection.html
- American Indian Cancer Foundation. Lung Cancer Screening.
https://americanindiancancer.org/aicaf-project/lung-cancer-awareness/
- American Lung Association. Native Americans and Lung Health.
https://www.lung.org/about-us/diversity-inclusion/native-american-heritage-month
- American Lung Association. What to Expect from a Lung Cancer Screening.
https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/screening-resources/what-to-expect-from-lung-cancer-screening
- Healthline.com. Can CT Scans Accurately Detect Lung Cancer? Last reviewed: June 16, 2022.
https://www.healthline.com/health/lung-cancer/how-accurate-is-ct-scan-for-lung-cancer
- Healthline.com. Race, Ethnicity, and Lung Cancer: An Expert Perspective on Improving Care. Last reviewed: November 19, 2020.
https://www.healthline.com/health/lung-cancer/race-ethnicity-and-lung-cancer
- Lungevity. Questions to Ask Your Healthcare Team.
https://www.lungevity.org/screening-for-lung-cancer/early-lung-cancer-screening/questions-to-ask-your-healthcare-team
- Medical News Today. What happens after you quit smoking? Last reviewed: November 19, 2018.
https://www.medicalnewstoday.com/articles/317956#outlook
- Memorial Sloan Kettering Cancer Center. Six Myths about Lung Cancer Screening: What You Need to Know. Last updated: November 2, 2020.
https://www.mskcc.org/news/six-myths-about-lung-cancer-screening-what-you-need-know
- The National Lung Screening Trial Research Team. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med. 2011;365:395-409.
- Truth Initiative. Tobacco use in the American Indian/Alaska Native community (fact sheet). 2020 May 28.
https://truthinitiative.org/research-resources/targeted-communities/tobacco-use-american-indianalaska-native-community
- US Centers for Disease Control and Prevention. American Indian and Alaska Native People and Cancer.
Last reviewed: January 30, 2023.
https://www.cdc.gov/cancer/health-equity/groups/american-indian-alaska-native.htm
- US Centers for Disease Control and Prevention. Lung Cancer Incidence in the American Indian and Alaska Native Population, United States Purchased/Referred Care Delivery Areas—2012–2016. Last reviewed: October 22, 2019.
https://www.cdc.gov/cancer/uscs/about/data-briefs/no14-lung-cancer-incidence-AIAN-PRCDA-2012-2016.htm
- US Centers for Disease Control and Prevention. What Are the Symptoms of Lung Cancer? Last reviewed: October 25, 2022.
https://www.cdc.gov/cancer/lung/basic_info/symptoms.htm
- US Preventive Services Task Force. Final Recommendation Statement – Lung Cancer: Screening. Last updated: March 09, 2021.
https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
- WebMD. Lung Cancer and Native Americans. Last reviewed: August 01, 2022.
https://www.webmd.com/lung-cancer/lung-cancer-and-native-americans
This slide show provides an overview of the importance of
early detection and screening for lung cancer in
Native Americans. Lung cancer is a leading cause of death from cancer among Native Americans. For Native Americans at high risk for lung cancer, screening can save lives – and the best time to get screened is before you feel sick. You can learn about the
symptoms that could be caused by lung cancer, the risks and benefits of lung cancer screening,
who is eligible for screening,
what happens during a lung cancer screening test (
low-dose CT scan), and
questions to ask your doctor about this procedure.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about lung cancer which will help other patients, caregivers and families.